Survivor Views: Patient Satisfaction by Gender
Overview
The American Cancer Society Cancer Action Network (ACS CAN) gives voice to cancer patients and survivors on critical public policy issues that affect their lives. As part of this effort, ACS CAN deploys surveys to better understand cancer patient and survivor experiences and perspectives, through our Survivor Views research panel. The panel is a group of cancer patients and survivors who respond to regular surveys and provide important insights to support ACS CAN’s advocacy work at all levels of government.
Fielded August 27-September 12, 2022, the latest survey explores cancer patients’ and survivors’ experiences with diagnosis and addressing their health concerns. The web-based survey was conducted among 1,236 patients and survivors nationwide diagnosed with or treated for cancer in the last seven years. The margin of sampling error associated with a sample of this size is +/-2.8% at a 95% confidence level.
Key Findings
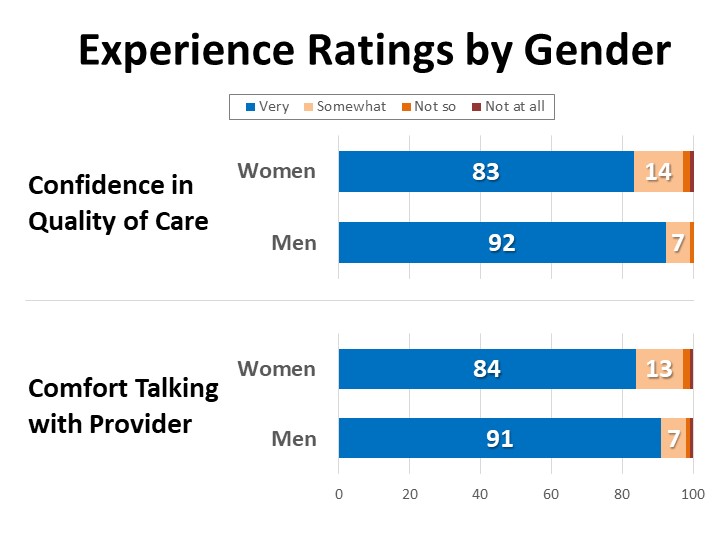
- Overall, the vast majority of cancer patients and survivors are very confident in the quality of their care and comfortable with their relationship with their provider, however women are about twice as likely as men to report feeling only “somewhat” confident in the quality of their care and “somewhat” comfortable in the provider relationship (13-14% vs. 7%).
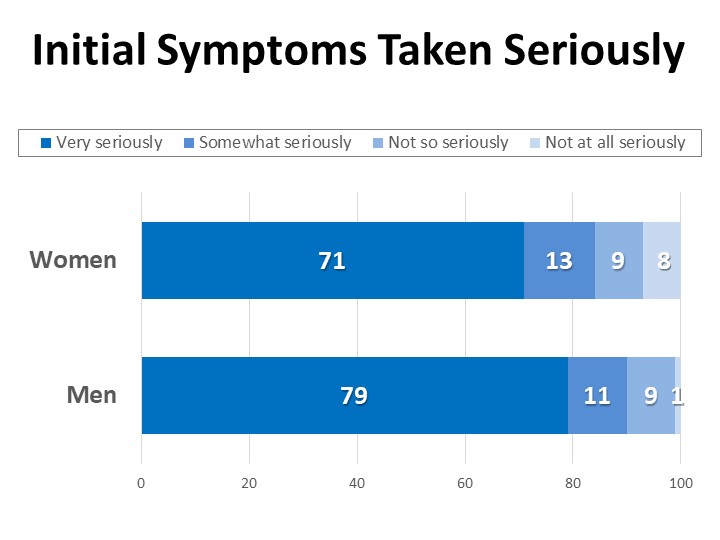
- While most interactions are positive, more than a quarter of those who were diagnosed after experiencing symptoms related to their cancer felt that their initial health concerns or symptoms were not taken “very” seriously. Women are more likely than men to report such experiences (31% vs. 21%).
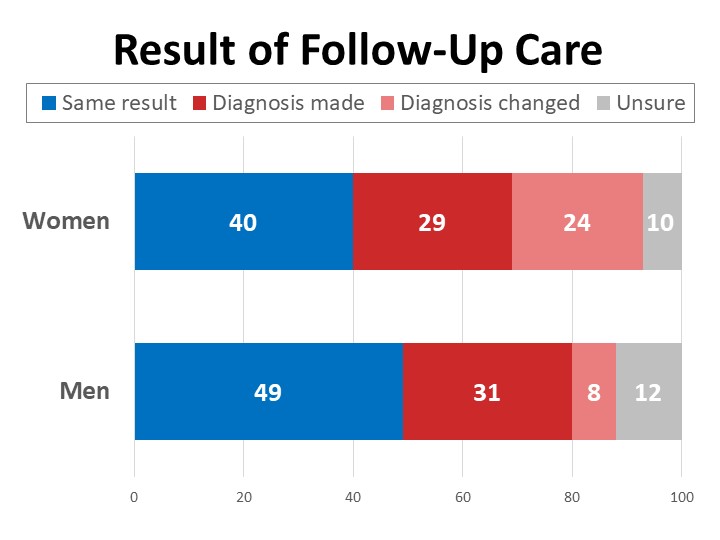
- One-third have sought additional care after feeling their initial concerns or symptoms were not taken seriously, and nearly half (48%) of those received their cancer diagnosis as a result of their self-advocacy and follow-up. Seventeen percent felt they needed follow up care but did not seek it due to concerns about cost or coverage.
Detailed Survey Findings:
Women Twice as Likely as Men to Report Middling Ratings of Their Experiences
Overall, the vast majority of patients (84%) are very confident in the quality of the care they have received from the primary provider responsible for their cancer care and treatment, and only 1% say they are “not at all” confident. However, among those giving middling ratings, women are more than twice as likely as men to say they are only “somewhat” or “not so” confident in the quality of their care (16% vs. 7%). Similarly, while the overwhelming majority (85%) are “very” comfortable talking with their provider about their diagnosis, treatment, or any concerns, women are twice as likely as men to report feeling only “somewhat” comfortable talking with their provider (13% vs. 7%).
Over One-Quarter of Those Diagnosed in Response to Symptoms Felt Initial Concerns Were Not Taken Seriously
One-third of survey respondents (33%) received their cancer diagnosis before noticing any symptoms, such as during regular screening or during treatment for another illness, and another fifth were diagnosed after the first time they discussed their symptoms with a provider. Thirty-one percent raised their symptoms with a provider two or more times before they received the attention that resulted in their diagnosis. A small number of respondents had to raise their symptoms five times or more before they received the care that led to their diagnosis, with women twice as likely as men to report this (6% vs 3%).
Among those who were diagnosed after experiencing symptoms (830n), more than a quarter of cancer patients and survivors (28%) felt their health concerns or symptoms were not initially taken “very” seriously by their provider. This includes those who say their concerns were taken “somewhat” seriously (12%), “not so” seriously (9%), and “not at all” seriously (7%). Women are more likely than men to report concerns being taken less than “very” seriously (31% vs. 21%), and 8% of women reported feeling their concerns were not taken seriously “at all” compared to just 1% of men.
Specific experiences related to not feeling concerns are taken seriously include feeling a provider ignored or dismissed symptoms (12%), having to advocate for tests a provider did not think were needed (11%), visiting multiple providers before concerns were taken seriously (9%), and feeling their pain was not taken seriously (7%). Experiences that are more commonly reported by women include feeling they had to “prove” their symptoms to an otherwise dismissive provider (8%) or having a provider suggest mental health support rather than medicine to treat their symptoms (3%).
Self-Advocacy Leads to Diagnosis for Nearly Half Who Previously Felt Dismissed
One-third of cancer patients and survivors have sought additional care, such as a second opinion, additional testing, or other follow-up, after feeling their health concerns or symptoms were initially disregarded or not taken seriously. Another 17% have at some point felt they needed such follow-up care but did not seek it due to concerns about cost or coverage, with women twice as likely as men to skip seeking additional care due to cost or coverage concerns.
Nearly half (48%) of those who sought additional care for themselves after initially feeling dismissed (404n) report receiving their cancer diagnosis or corrected cancer diagnosis as a result of their self-advocacy and follow-up. Women are three times as likely as men to report their diagnosis changed as a result of the additional care they sought after feeling their initial concerns were not taken seriously.
Over 400 survey respondents shared personal accounts of their experiences feeling that their symptoms or concerns were initially disregarded or not taken seriously. Many of these stories also reflect obstacles related to cost and coverage, challenges getting appropriate screening, and having to enlist outside help in order to get the care that led to their diagnosis:
“I felt no one wanted to help me because I was uninsured. I went to multiple doctors and even 3 different hospitals and no one did any testing at all until my friend’s wife took me to a 4th hospital and they diagnosed and treated me.”
“Because I'm normally a healthy person, my providers ignored my severe pain as muscle spasms. I went through pain killers, therapy, massage and all kinds of useless therapies seeing multiple doctors before I finally lost my temper and demanded an MRI and CT scan. It took 8 months of almost monthly visits to my PCP, orthopedic surgeons and therapists to finally get a diagnosis.”
“My initial provider made excuses for my symptoms. I insisted on screening colonoscopy as it was time. She said since my last one 5 years previously was normal, I could wait another 5 years. My response was that if she didn’t order it I would find someone who would. She did. It was cancer.”
“Emergency room doctors thought I was seeking pain meds. Two weeks later I returned, this time by ambulance. The emergency doctor reluctantly sent me for another MRI, which showed a fractured L1 vertebrae which was a result of Stage IV breast cancer.”
“I began seeing my PCP over a year before I was diagnosed with stage III cancer. I was told to reduce my stress and follow up. I was told by a neurologist that what I was experiencing was ‘deep-seated depression manifesting physical symptoms’ and that I should attend therapy and possibly take anti-depressant medication. As a busy working woman in my 30's I feel all of my symptoms were dismissed because I didn't fit the mold of what cancer looked like.”
“I did not have the money to go get a sonogram and a mammogram. I had a second opinion and the tumor had grown so fast. It was very stressful, my journey. I realized that when you get cancer no one cares. They care if you have the money to pay. If you don't they make you wait.”
“My doctor did not believe me when I felt a pain in my breast. He put his hand on my knee and told me to smile when I became upset. It wasn't until I met my new oncology team that I felt supported or heard.”
“I was going to a free clinic. Had to keep going, seeing a different doctor each time, until finally one put me in for a colonoscopy. Doctors really need to listen to patients.”
Over a quarter of respondents report feeling they needed to ask someone else, such as a family member, friend, or someone who works in health care, to help them talk with a provider about their health concerns or to help advocate on their behalf in order to be taken seriously. Black patients and survivors are most likely to report feeling they needed to ask someone else to help advocate for them on their behalf (29%). These results illustrate an important potential benefit of patient navigation, which 98% of the Survivor Views cohort have previously agreed is important for cancer patients to have access to.
Methodology
ACS CAN’s Survivor Views research initiative was designed to enhance the organization’s mission to end suffering and death from cancer. Data provided by cancer patients and survivors as part of this project allows for a greater understanding of their experiences and opinions on cancer-related issues and gives voice to cancer patients and survivors in the shaping and advocating of public policies that help prevent, detect, and treat cancer and promote a more positive quality of life for those impacted.
To ensure the protection of all participants in this initiative all research protocols, questionnaires, and communications are reviewed by the Morehouse School of Medicine Institutional Review Board.
The survey population is comprised of individuals who meet the following criteria:
- Diagnosed with and/or treated for cancer within the last seven years
- Over the age of 18 (parents of childhood cancer survivors were invited to participate on behalf of their minor children)
- Reside in the US or US territories
Potential Survivor Views participants were invited to participate through email invitations, social media promotion, and partner group outreach. Those who agreed to participate after reviewing the informed consent information completed a brief survey including demographic and cancer history information to inform analysis as well as topical questions as discussed in this document. The data were collected between August 27-September 12, 2022. A total of 1,236 cohort participants responded to the survey, providing a margin of error of +/-2.8 percentage points at a 95% confidence level.
About ACS CAN
The American Cancer Society Cancer Action Network (ACS CAN) makes cancer a top priority for policymakers at every level of government. ACS CAN empowers volunteers across the country to make their voices heard to influence evidence-based public policy change that improves the lives of people with cancer and their families. We believe everyone should have a fair and just opportunity to prevent, find, treat, and survive cancer. Since 2001, as the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate, ACS CAN has successfully advocated for billions of dollars in cancer research funding, expanded access to quality affordable health care, and advanced proven tobacco control measures. We’re more determined than ever to stand together with our volunteers to end cancer as we know it, for everyone. For more information, visit www.fightcancer.org.