New State Law Takes Effect July 1, 2022
Indiana lawmakers recently passed HEA 1238, which requires most private insurance plans to provide coverage for all preventive colorectal screenings for individuals aged 45 and older, including colonoscopies that follow an abnormal stool-based test.
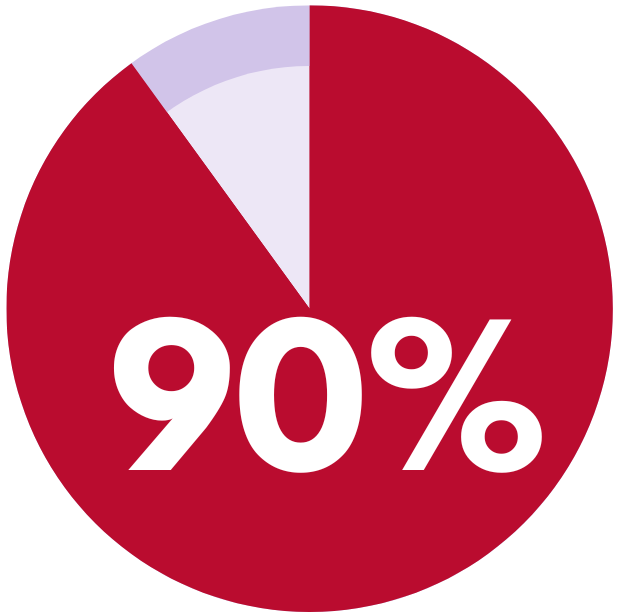
When given the choice by a provider, many average-risk patients prefer a stool-based test over colonoscopy and, nationally, about 10 percent of eligible patients opt for stool-based testing.
The new law – which covers about 2.5 million covered lives in private insurance plans – combined with recent federal guidance on coverage of follow-up colonoscopies, will ensure that more Hoosiers who opt for stool-based testing and receive an abnormal result can also complete a follow-up colonoscopy without facing burdensome cost-sharing.
By the Numbers: Colorectal Cancer in Indiana
3,000Number of Hoosiers diagnosed with colorectal cancer in 2021 |
1,160Number of Hoosiers who died from colorectal cancer in 2021 |
68%Percentage of Hoosiers up-to-date on their colorectal screenings |
|
Percent decline in colonoscopies and biopsies performed in the spring of 2020 |
4.5KProjected excess colorectal deaths in U.S. over 10 years due to lower screening rates |
Frequently Asked Questions
 Aren't preventative colorectal screenings already covered?
Aren't preventative colorectal screenings already covered?
Health plans regulated by the ACA are required to cover preventative cancer screenings without cost-sharing. However, some patients who take a stool-based test may require a follow-up colonoscopy if their stool-based test has an abnormal result. Some insurance plans require patients to pay a copay or coinsurance for the follow-up colonoscopy which discourages patients from completing the screening. HEA 1238 and new federal guidance from the Department of Labor should ensure this barrier is removed for more patients.
 Why offer stool-based options first instead of colonoscopy?
Why offer stool-based options first instead of colonoscopy?
Stool-based tests are often easier for patients to complete than a more invasive and time-consuming colonoscopy. Patients can complete the stool-based test at home and on their own schedule. Stool-based tests are also effective, typically up to 92 percent accurate at detecting colon cancer. When given the choice, many average-risk patients prefer a stool-based test over colonoscopy [2] and, nationally, about 10 percent of eligible patients opt for stool-based testing at home [3].
 How many other states have passed legislation?
How many other states have passed legislation?
At least seven states, including Kentucky, have eliminated cost-sharing for follow-up colonoscopies after an abnormal stool-based test. Similar action is pending in several other states.
How do I know if my or my patient’s insurance plan covers follow-up colonoscopies?
The new state law combined with recent federal guidance should ensure most insured patients now have access to follow-up colonoscopies without cost-sharing, but patients should call their insurance carrier to verify that colonoscopies after an abnormal stool-based test are covered.
[1]https://www.mdsave.com/procedures/colonoscopy/d783fdcd/indiana#:~:text=O... 0MDsave%20works. Accessed October 22, 2021
[2] https://www.aacr.org/about-the-aacr/newsroom/news-releases/average-risk-.... Access October 22, 2021
[3] American Cancer Society. Cancer Prevention & Early Detection Facts & Figures, 2021-2022. Atlanta: American Cancer Society; 2021.